Summary: Researchers analyzing postmortem brain tissue found two types of altered cells in people with depression: excitatory neurons, which control mood and stress, and microglia, which control inflammation. These findings highlight how depression is linked to measurable changes in the brain, not just emotional symptoms.
By mapping gene activity and DNA regulation, scientists have identified cellular changes unique to depression. This breakthrough could lead to cell-specific treatments, offering hope for the millions of people around the world who suffer from depression.
Key facts
- Target cell types: Mood-related excitatory neurons and inflammation-regulatory microglia show altered gene activity in depression.
- Rare resources: The study used brain samples from the Canadian Douglas Bell Brain Bank, one of the few banks that have been donated by people with psychiatric disorders.
- Treatment potential: Identifying these cells paves the way for targeted treatments for depression.
Source: McGill University
Scientists at McGill University and the Douglas Institute have discovered two distinct types of brain cells that show changes in individuals suffering from depression.
The research, published in Nature Genetics, paves the way for the development of new treatments that target these cells. It also sheds light on depression, a leading cause of disability worldwide, affecting more than 264 million people.
“This is the first time we have been able to identify, by mapping gene activity with mechanisms regulating the DNA code, which specific types of brain cells are affected by depression,” said lead investigator Dr. Gustave Toureci, a McGill professor, clinical scientist at the Douglas Institute and a Canada Research Chair in Major Depression.
“This gives us a clear picture of where the changes are occurring and which cells are involved.”
A rare brain bank makes a breakthrough possible.
The researchers used postmortem brain tissue from the Canadian Douglas Bell Brain Bank, one of the few collections in the world with tissue donated by people with psychiatric disorders.
They used single-cell genomic techniques to analyze the RNA and DNA of thousands of neurons, identifying which cells function differently in depression and which DNA sequences might explain these differences. They studied samples from 59 people with depression and 41 people without depression.
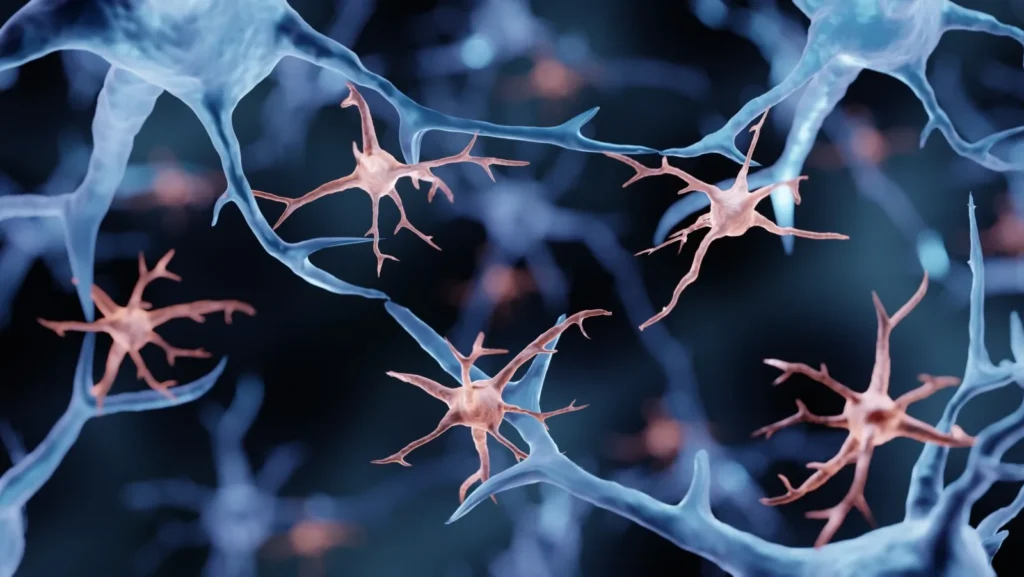
The results revealed gene activity in a specific type of excitatory neuron involved in regulating mood and stress, and in a subtype of microglia cells that help regulate inflammation. Many genes in both types of cells function differently in people with depression, suggesting possible changes in these important brain systems.
By identifying brain cells affected by depression, the research provides new insights into its biological basis and, more broadly, challenges persistent misconceptions about the disorder.
“This study confirms what neuroscience has been teaching us for years,” says Torecki. “Depression is not just emotional; it reflects real, measurable changes in the brain.” For decades, mental health conditions like depression were often misunderstood as purely psychological or emotional in nature—intangible states that could not be easily linked to the biological workings of the brain. However, advances in neuroscience have steadily revealed that mental illnesses are rooted in concrete changes to brain structure and function. This latest research adds to that growing body of evidence by identifying specific cell types that are altered in people with depression, emphasizing that the disorder is deeply biological in origin.
The findings underscore the importance of treating depression not merely as a mood disorder but as a condition with underlying neurobiological mechanisms that can be observed, measured, and potentially targeted for treatment. By pinpointing the exact brain cells involved, researchers can develop more precise therapies aimed at restoring healthy brain function. This marks a crucial shift in how depression is perceived—not as a personal weakness or purely emotional struggle, but as a legitimate medical condition involving identifiable and treatable changes in the brain.
In the next step, the researchers want to investigate how these cellular changes affect brain function and whether addressing them could lead to better treatments.
About this neuroscience and depression research news
Author: Keila DePape
Source: McGill University
Contact: Keila DePape – McGill University
Image: The image is credited to Stackzone Neuro
Original Research: Closed access.
“Single-nucleus chromatin accessibility profiling identifies cell types and functional variants contributing to major depression” by Anjali Chawla and Gustavo Turecki et al. Nature Genetics.
Abstract
Single-nucleus chromatin accessibility profiling identifies cell types and functional variants that contribute to major depression.
Genetic variations associated with major depressive disorder (MDD) are high in the regulatory genome.
Here we investigated genetic regulatory mechanisms underlying MDD compared with neurotypical controls by combining chromatin accessibility in single cells with gene expression in over 200,000 cells from the dorsolateral prefrontal cortex of 84 individuals.
Major depressive disorder (MDD) is increasingly being understood through the lens of molecular and cellular neuroscience, and recent findings provide compelling evidence of chromatin-level alterations in specific brain cell populations. In deep layer excitatory neurons, researchers observed MDD-associated changes in chromatin accessibility—regions of the genome that become more or less open to transcriptional activity. These changes were marked by increased accessibility to specific transcription factor (TF) motifs, particularly those bound by NR4A2, a stress-responsive, activity-dependent transcription factor. This suggests that these neurons are undergoing molecular changes that directly impact their function, possibly altering how they process stress and regulate emotional behavior. Notably, these same neurons were found to be enriched with genetic variants linked to MDD, many of which appear to affect transcription factor binding sites tied to genes that regulate synaptic communication, a key process implicated in mood regulation and cognitive function.
In addition to neurons, the study identified crucial alterations in non-neuronal cells, particularly microglia—the brain’s resident immune cells. A distinct subset of microglia located in the gray matter of individuals with MDD showed reduced accessibility to transcription factor binding sites involved in maintaining immune homeostasis. This suggests a disrupted ability to regulate immune responses in the brain, which may contribute to the neuroinflammatory processes increasingly associated with depression. Together, these findings highlight a complex interplay between genetic risk, neuronal activity, and immune dysregulation in MDD. They also reinforce the view of depression as a disorder rooted in tangible, cell-specific biological changes, opening the door to more targeted, mechanistic approaches for diagnosis and treatment.
Finally, we identified genetic regulatory effects of MDD risk variants using sequence-based accessibility predictions, donor-specific genotypes, and cell-based assays.
These findings shed light on the cell types and regulatory mechanisms through which genetic variation may increase the risk of MDD.